
Ankle arthritis — degenerative-dystrophic damage to cartilage tissue. But because as the disease progresses, the joint surfaces of the bones are also involved in this process, so it is more correct to call it osteoarthritis. In foreign literature, when describing this disease, the term osteoarthritis is used, which denotes not only degenerative changes, but also inflammation against this background.
Osteoarthritis — This is a chronic, progressive joint disease in which cartilage, the articular surfaces of bones, the joint capsule and periarticular tissues are destroyed. This leads to pain and impaired joint mobility. The ankle rarely gets osteoarthritis, unlike the knee. The disease occurs more often in women over 50 years of age and in athletes with leg injuries. For ankle arthritis, treatment depends on the manifestations of the disease and is selected individually by the orthopedic surgeon. Doctors use methods proven to be effective and safe, and practice a multidisciplinary approach to treat the problem and prevent the progression of joint disease.
This article is for advisory purposes only. Treatment is prescribed by a specialist after consultation.
How does the disease develop?
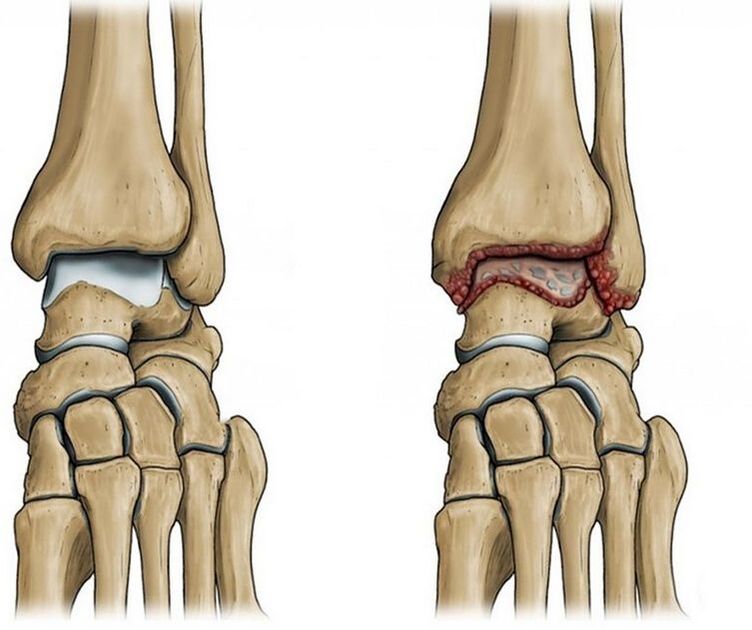
The ankle joint is formed by three bones: the tibia, fibula and talus, covered by a joint capsule and reinforced by ligaments. Thanks to the action of the muscles, the foot contracts and stretches. Normally, joint surfaces are smooth and slide easily relative to each other during movement. Covered with a dense, elastic layer of cartilage, its main function — protecting bones and absorbing loads. The joint cavity contains synovial fluid. It plays the role of intra-articular lubrication, preventing friction of joint parts and their wear during movement.
But due to injury or natural aging of the joint, the joint surface becomes rough and the cartilage tissue loses its smoothness and elasticity. When the cartilage is damaged and degeneration occurs, the bones begin to come into contact with each other when moving in the joint, accompanied by pain.
In an effort to "protect" and to compensate for further damage to the joint and surrounding tissues, bone spurs are formed — growing along the edges of the bone's articular surface. As a result, joint mobility is partially or even completely limited.
Depending on the cause of the disease, people distinguish the following types of osteoarthritis:
- Primary or idiopathic osteoarthritis. In this case we are talking about degenerative-dystrophic changes in the joints
- Secondary is related to exposure to a specific causative factor, usually a previous joint injury. And this form is most often diagnosed
Risk factor
The main factors influencing the development of ankle arthritis:
- Injuries in and around joints, such as fractures, tears, and ligament ruptures
- Ankle surgery
- Past arthritis damage
- heavy loads: professional sports, ballet, long walks, work that involves long periods of "standing on your feet"
- sedentary lifestyle
- wearing high heels for long periods of time
- overweight
- Hereditary collagen diseases lead to impaired collagen synthesis
- Chronic injuries to joint structures due to excessive loading
- Metabolic disorders: diabetes, gout
- Estrogen deficiency in postmenopausal women
- Rheumatism
- foot deformities, such as flat feet
- degenerative-dystrophy of the spine, complicated by the formation of hernias between the vertebrae, accompanied by nerve root compression
Ankle arthritis: symptoms
Key signs of joint disease — Pain is what makes you seek help from a doctor. At the beginning of the disease, the pain is only unpleasant after prolonged exercise and gradually subsides with rest.
Depending on the stage of pathological changes in the joints, the pain becomes more intense and lasts at rest and even at night. Other symptoms occur.
There are three stages of the disease:
- The first stage is characterized by mild swelling, redness of the skin in the joint area, pain in the afternoon or after intense exercise. The discomfort is localized along the front of the foot, along the joint line, and moves to the lateral aspects of the ankle. Foot X-rays may not show any changes yet.
- In the second stage, the pain becomes constant, a crunching sound appears when moving the joint, mobility is limited, and the joint "gets stuck". When examined on X-ray films, growth can be noticed along the edges of the articular surfaces of the bones: tibia, ankle and talus, as well as a narrowing of the joint space
- In the third stage, the joint is deformed, which is why only low-amplitude, swinging movements are possible. X-rays show that the bones have grown large, the joint space is clearly narrowed or even absent. Due to joint instability, patients often twist their legs, which only aggravates the condition with sprains, torn ligaments, and general deterioration.
Pain caused by ankle arthritis has characteristic characteristics:
- The maximum level is indicated at the beginning of movement — the so-called onset of pain
- Increases significantly under load, especially when running and jumping
- Usually appears in the evening, at night or immediately after waking up
Due to pain, the foot has limited movement as well as gets stuck in the joint, causing the cartilage to be destroyed.
Symptoms appear episodically: periods of exacerbation alternate with periods of remission. With a more severe condition, the symptoms are more pronounced. During remission, symptoms gradually decrease and may even disappear completely.
Which doctor should I contact?
If you have pain and stiffness when moving your ankle, you should consult an orthopedic surgeon. If another cause of joint discomfort is identified, consultation with a neurologist, rheumatologist, or endocrinologist may be necessary.
Diagnose
To make a diagnosis, the doctor clarifies the complaints, specifies the time when the pain occurred, which contributed to its appearance and intensification. The specialist collects data on existing diseases, injuries and lifestyle characteristics, conducts an examination, evaluates the range of motion of the joints and performs diagnostic tests.
On the basis of the information received, a diagnosis can be made, but for confirmation and appropriate treatment planning, additional examination methods are needed, which may include:
- X-rays of the ankle joint are of primary importance in diagnosing and determining the stage of disease development. Imaging shows narrowing of the joint space, bone spurs at the edge of the bone's joint surface, cysts, and signs of osteoporosis located under the cartilage.
- CT arthrography reflects more detailed images. The doctor can evaluate in detail the condition of the patient's bone structure and cartilage tissue
- MRI is used to study cartilage and soft tissue
- Joint ultrasound evaluates the condition of the soft structures of the joint
Treatment of arthritis
Treatment of the pathology is long-term and is carried out under the supervision of an orthopedic traumatologist on an outpatient basis. How to treat arthritis in the legs depends on the stage of damage and existing complications.
The main goal of treating the disease in a modern clinic is to reduce leg pain, improve the patient's quality of life and slow down the progression of joint disease. To do this, the doctor develops a series of therapeutic and preventive measures, pharmacological and non-pharmacological, and adjusts the patient's lifestyle.
Adjust lifestyle and nutrition
Adequate physical activity and nutritional adjustments will help limit degenerative changes. After the examination, the clinic's doctors can give recommendations on how to lose weight as well as optimize the load on the legs.
Treatment medicine
Medicines are selected individually, based on examination data, symptoms and comorbidities. Patients may be prescribed:
- Analgesic. Usually these are non-steroidal anti-inflammatory drugs in the form of tablets, gels, injections to relieve pain and inflammation
- Antidepressants and anticonvulsants in cases of long-lasting, severe, difficult-to-treat pain
Exercise therapy
Specially selected exercises help maintain joint range of motion, reduce pain and limit the progression of degenerative changes. The patient performs the recommended exercises at first under the supervision of a specialist, then — alone, at home.
Massage
Massage of the lower limbs helps normalize the nutrition of joint tissues. It is prescribed outside the acute phase. During the training session, the specialist performs passive movements in the joints, helping to prevent muscle contractures and joint stiffness.
Support equipment
Special orthotics, canes, and walkers may be recommended to reduce stress and stabilize the ankle joint.
Surgery
It is only used in cases where articular cartilage is seriously destroyed and joint mobility is limited. After surgery is a long period of rehabilitation and conservative treatment. Arthroscopy or arthroplasty in the later stages of ankle arthritis — is practically the only chance to avoid disability and preserve joint mobility.
Why is ankle arthritis dangerous?
Changes that have formed in the joints are irreversible. Therefore, treatment is aimed at slowing down the pathological process in order to maintain the patient's ability to work and quality of life. Such goals can only be achieved with timely treatment and strict adherence to the doctor's recommendations.
As arthritis develops, a pronounced deformity of the joint is formed. The range of motion is sharply reduced, as a result, support of the foot becomes difficult, walking without crutches or a cane is almost impossible.
Chronic, constant pain in the joints leads to anxiety and depressive disorders.
Prevent
Prevention of joint disease includes the following measures:
- Avoid activities that cause injury. For example: jumping from a great height, running
- Avoid injury
- Be careful in icy conditions, wear non-slip shoes
- Control your body weight
- Normalizing body weight will help reduce stress on the ankle joints
- Maintain moderate activity
- An inactive lifestyle is dangerous and leads to complications, as well as overuse and excessive microtrauma
- Keep your joints healthy
- Consult your doctor promptly and treat musculoskeletal diseases
Key points from the article:
- The rate of degenerative and dystrophic foot disease is 87%
- Occupational hazards, daily habits, and past injuries can lead to ankle arthritis.
- A common symptom of joint disease — pain, accompanied by a crunching sound when moving, local swelling and then limited movement of the foot
- Treatment for ankle arthritis is typically conservative and includes both pharmacological and non-pharmacological approaches.
- Progressive ankle arthritis leads to disability and complete loss of foot function

























